Infection Control
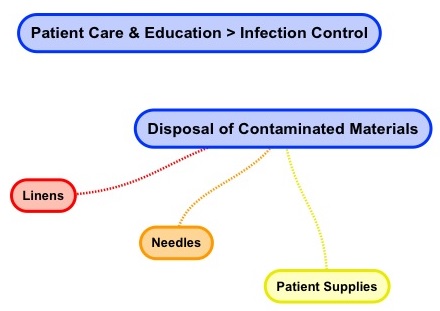
Home > Patient Care And Education > Infection Control
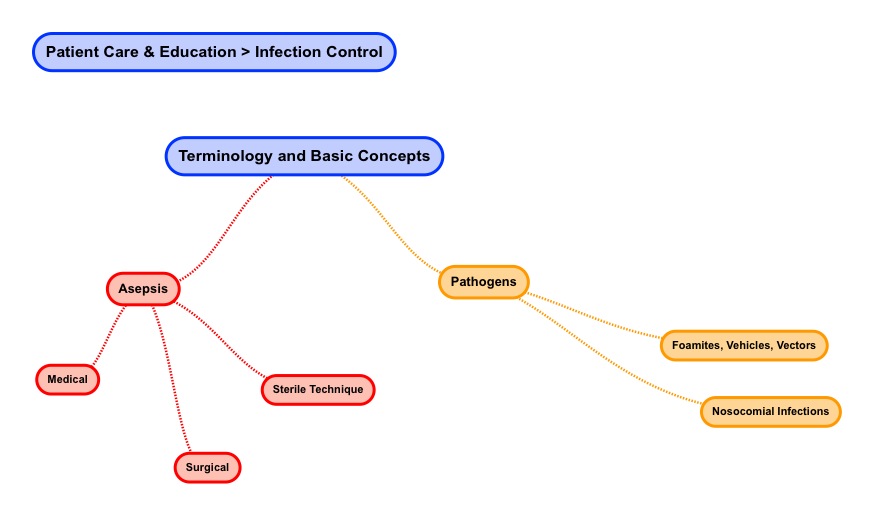
- Terminology and Basic Concepts
- Cycle of Infection
- Standard Universal Precautions
- Additional or Transmission Based Precautions
- Disposal of Contaminated Materials
Seven; 7 questions out of the 30 questions in the Patient Care and Education content area come from the Infection Control sub-topic.
Can we please get your advice on this one question?
- Terminology and Basic Concepts
When it comes to reviewing the topic of infection control it is useful to review some basic terminology as well as concepts.
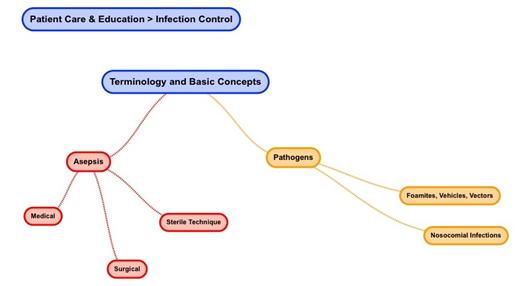
The terms sepsis means whole-body contamination. When we add the letter “a” in front of sepsis it becomes asepsis and the word’s meaning changes. Asepsis is a term which means being free from disease-causing contaminants.
In all of health care including radiation therapy, our first mandate is help patients and certainly not to “harm” to patients. In support of this aim, we as health care workers are charged with providing patient’s a safe environment. A safe environment means a medical, surgical, as well as sterile technique context which is clean and does not contain disease. The objective is to help patients improve their overall health outcome and not to bring them into a health care environment containing disease-causing contaminants.
- Medical Asepsis
The term medical asepsis refers to the health care process of protecting against infection by removing pathogenic microorganisms. Infectious agents consist of: pathogens including bacteria, viruses, and fungi that normally live in skin as well as mucous membranes. The health care context caters to both patients as well as a variety of infectious agents.
Medical asepsis involves stopping infectious agents from causing harm to patients as well as health care workers. http://www.mercycares.com

Here are some examples of medical asepsis:
- Clean contaminated objects and (this reduces the number of organisms)
- Hand washing (this reduces the number of organisms)
- Perform disinfection as well as sterilization (this inactivates organisms)
- Use antiseptics (this inhibits organism growth)
Medical asepsis therefore involves reducing the number as well as the spread of infectious agents.
- Surgical Asepsis
The term surgical asepsis means the complete removal of microorganisms including spores from an object.
Surgical asepsis involves first cleaning an object and then second sterilizing the object. The idea is to produce an object which is free of microorganisms and spores. Surgical asepsis is required for any invasive (penetrating body tissues) medical procedure. http://profstelmark.com/ppi/Surgical%20Asepsis%202.ppt

Here are some examples of invasive medical procedures that would require medical asepsis:
- Catheterization of the urinary bladder
- LDR prostate seed implant
- Placement of HDR tandem and ring
- Dressing changes
- Tracheostomy care
- Surgery of any kind
Proper health care attire is required for surgical asepsis. Common attire includes: scrubs, gown, cap, mask, gloves, as well as shoe covers.
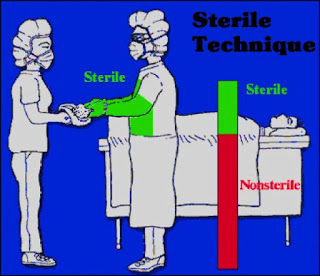
- Sterile Technique
The term surgical technique refers to how a health care worker implements surgical asepsis.
Here are some examples of sterile technique in relevant to radiation therapy. So, the way in which a health care worker puts on sterile gloves is sterile technique. The way in a radiation therapist sterilizes LDR prostate implant seeds is sterile technique. The way in which a radiation oncologist places a HDR tandem set is sterile technique.

The sterile technique notion here is to act or behave in logical ways to ensure the absence of viable pathologic organisms when involved in invasive medical procedures. There are for example specific ways to put on sterile gowns, sterile gloves as well as specific ways to handle as well as transfer surgical instruments to preserve a sterile field. http://www.uofmmedicalcenter.org

A sterile field is an area or open space like a sterile towel within a tray which is considered free of microorganisms.
As we continue our review of infection control it is useful to define some terms.
- Pathogen
A pathogen can be defined as something that causes a disease. In other words, a pathogen is an infectious agent. http://www.sciencedaily.com. The following organisms (by way of example) have the ability to carry infection: protozoan, bacteria, fungi, as well as viruses.
- Fomite
A fomite is simply defined as an inanimate (not living) substance or an object capable of carrying infectious agents. http://www.microblogology.com/?p=961 Examples of inanimate objects which are capable to transmitting infection are utensils, toilet seats, hair brushes, towels, as well as a water fountain.
- Vehicle
In terms of infection control, the term vehicle or
vehicle-borne is used to describe an indirect transmission of infectious
agents. Examples of vehicles or agents capable of acting in indirect transmission
include: water as well as food.
- Vector
A vector is something that is animate (or living) which is an agent carrying infection. People, animals, as well as microorganisms are vector examples. http://www.cdc.gov/ncezid/dvbd/ . This infection is usually carried out through feeding activity. Specifically, vectors examples would include rats as well as blood-sucking insects like: mosquitos, ticks, fleas, and mites.
- Nosocomial Infection
The term nosocomial infection or HAI (Health Care Acquired Infection) refers to an infection acquired in a health care or hospital setting. These infections may be acquired from other patients, hospital staff, as well as contaminated objects in the health care environment.
These infections may occur within 2 days after a patient’s admission into a health care setting till 3 days after discharge or even 30 days after a surgery. http://ceaccp.oxfordjournals.org/content/5/1/14.full . Some 10% of patients acquire a nosocomial infection or around 2 million patients a year get an infection. Of these infections, some 20,000 deaths occur in the United States each year.
Common infection sites include the urinary tract, surgical sites, the respiratory tract, gastrointestinal tract, skin, as well as the central nervous system.
- Cycle of Infection
As we continue to review of infection control, an understanding of the: cycle of infection is relevant. The cycle of infection consists of four main parts; namely, pathogen, source or reservoir of infection, susceptible host, and method of transmission.
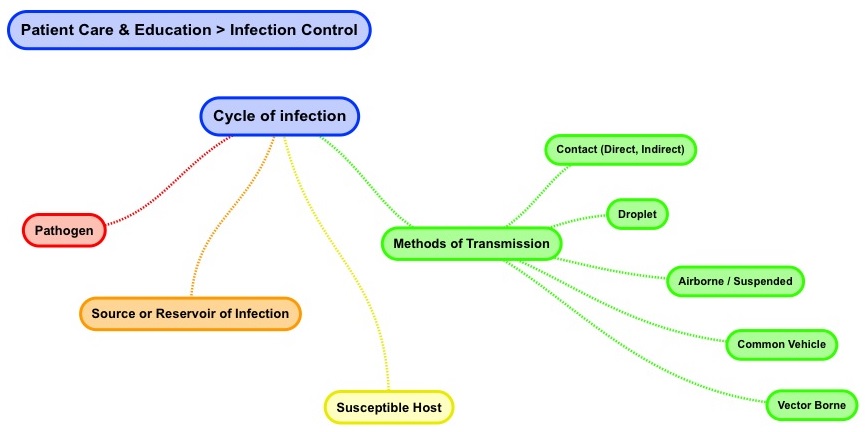
Pathogen
A pathogen can be defined as something that causes a disease. In other words, a pathogen is an infectious agent.
The following organisms (by way of example) have the ability to carry
infection: protozoan, bacteria, fungi, as well as viruses.
Here are some clinical examples of pathogens. Bacterium examples are: bacterial meningitis and strep throat. Virus examples include hepatitis, A, B, and C. A fungus example is mycosis fungoides which is a cutaneous T-cell lymphoma.
The body’s immune system destroys most pathogen before they can affect us.
- Healthcare workers as well as patients are considered exposed when we come in contact with pathogens.
- Healthcare workers as well as patients are considered infected when pathogens enter the body and subsequently result is disease.
Three factors affect if exposure results in infection; these are, dose, virulence, and resistance. Dose refers to the amount of pathogens a body is exposed to and the amount of pathogens entering a body. Virulence refers to the activity or strength of the organism. Resistance refers to the extent that the exposed person’s immune system can fight the infection.
Source or Reservoir of Infection
A reservoir is a holding place. This (reservoir) holding place is home to the source of infection. The reservoir is a place where a pathogen can (grow up) thrive and survive. A source may be inanimate (not living) as well as animate (living). Inanimate source of infection examples are fomites like table tops and door handles. Animate source of infection examples are human beings as well as animals.
People are susceptible to other human reservoirs. Strep throat, measles, mumps, as well as sexually transmitted diseases are examples of where one person acts as a reservoir or source of infection affecting another person with whom they have contact.
People are susceptible to animal reservoirs as well. Here are some animal to people infection examples. Malaria comes from mosquitos. Anthrax comes from sheep. Swine flu comes from pigs. And, rabies comes from mammal (dog, bat, raccoon, and so on) bites. https://www.cdc.gov/
Susceptible Host
A susceptible host is a person who can’t resist the pathogen (infectious agent) invading their body. The susceptible host’s inability to resist the pathogen may be due to only one or a combination of three factors. The dose (amount of exposure), and / or the virulence of the pathogen, and / or the susceptible host’s compromised immune system means the exposed individual end up with an infection. The host is susceptible and is overcome by the pathogenic microorganism.
Methods of Transmission
There are various methods of transmission. For the purpose of this review we categorize them as follows: contact (direct), contact (indirect), droplet, airborne / suspended, common vehicle, and vector borne.
Direct contact transmission involves a body surface to body surface transfer of microorganisms and infectious agents. Examples of skin to skin transmission are chicken pox as well as “pink eye” or conjunctivitis.

Indirect contract transmission involves a body surface and an intermediate object (a fomite) including the air. The body surface comes in contact with a substance or an object capable of carrying the infectious agent. Skin to substance transmission may occur when a healthy person uses a dirty glass a sick person previously used. Skin to substance transmission may also occur when a healthy person contracts measles by sitting on tables and eating where a sick person previously ate.
Droplet (or moisture) transmission occurs when droplets containing microorganisms find their way into contact with a healthy person. One example of droplet transmission is fecal-oral contamination, where feces in a pool or water park water come into contact with health people. Another example of droplet transmission involves close respiratory contact. This close respiratory contact means that a healthy person can easily inadvertently inhale droplets in a sick persons cough.

Airborne / suspended transmission means that pathogens or infectious agents are transmitted by air. A common airborne transmission example is tuberculosis. Another airborne infectious agent example is herpes zoster (before lesions are crusted over).
Common vehicle transmission refers to a medium or mode of infection (be that food, water, or blood) that tends to be commonplace. Syphilis as a common vehicle transmission example that tends to be sexually transmitted disease. Another common vehicle transmission example is cholera which tends to be transmitted in contaminated water.

Vector borne transmission refers to an infectious agent transmitted directly into the susceptible host’s blood stream. Vectors acquire an infectious agent (microbes) by feeding. For these microbes the vector is a reservoir in which to multiply. Transmission occurs when vectors engage in blood sucking thereby sending microbes to the susceptible host. Blood sucking insects include mosquitos, flees, as well as lice. Blood sucking arachnids include mites as well as ticks.
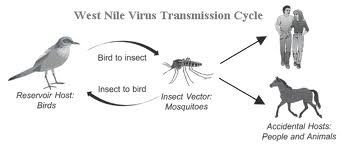
The above diagram shows how mosquitos (a vector) transmit disease
- Standard Universal Precautions
Standard Universal Precautions is a medical practice which says that health care workers should avoid general patient contact with blood, body fluids, as well as non-intact skin. All patients are considered possible sources of pathogens or infectious agents. So, avoiding contact with possible infectious agents reduces the transmission of pathogens. http://www.cdc.gov/hicpac/pdf/isolation/Isolation2007.pdf
Infection
control precautions consist of the use of hand washing, personal protective
gear, as well as assuring a medical environment which is clean of
contamination. We will review standard
methods of precaution which include hand washing, use of gloves & gowns,
use of mask & face shields, as well as medical asepsis.
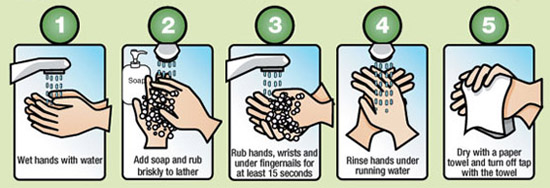
Hand Washing
Hand
hygiene us a major part of standard universal precautions and represents an
effective way to prevent the transmission of health care related infectious
agents.
The World Health Organization recommends that hands be washed as follows (http://www.who.int/csr/resources/publications/EPR_AM2_E7.pdf) :
- Before and after any direct patient contact
- Immediately after gloves are removed
- Before handling any invasive equipment
- After touching blood, body fluids, as well as non-intact skin
- After
contact with inanimate objects (fomites) in the vicinity of the patient
When it comes to hand washing steps, the process is well established. The points to keep in mind are that:
First, you need to use mechanical action (rub your hands together and not just run your hands under water) Second, you need to wash your hands for sufficient time.
http://www.simcoemuskokahealth.org
Gloves
The use of clean non-sterile gloves is a standard practice. Use gloves if there is any chance of encountering contaminated surfaces, patient blood, body fluids (for example mucous & secretions), as well as non-intact skin (for example wounds or bandages). Using gloves helps protect the health care worker as well as the patient from any inadvertent transmission of pathogens (infectious agents).

Gloves need to be changed if they are torn or punctured. Wash hands after the removal of gloves.
http://www.health.state.mn.us/divs/idepc/dtopics/infectioncontrol/ppe/comp/gloves.html
Gowns
The
use of a clean non-sterile gown is considered a standard patient handling
intervention. Gown use is applicable to cases where the health care worker
comes into skin to skin contact with a patient or with objects (fomites) which
have come into contact with infection.
The above gown use application is very wide and would indicate that gown use should be widespread and apply to all patient handling. To gown or not to gown is the topic of many standard precaution recommendations.

In
pragmatic terms, gown use is suggested for all acute care health care contexts
where patient immunity is compromised. Gown use is also suggested in all
contexts where patients are known to possess infectious agents and where there
is likelihood that contact with a patient or with objects (fomites) which have
come into contact will result in pathogen transmission. If in doubt use a gown.
Masks
Minimum
infection prevention precautions include the use of a mask. A mask is sometimes
also called a surgical mask. A mask covers the nose as well as mouth protecting
mucous membranes from exposure to body fluid sprays or splashes.
Wearing a mask (by a patient and / or a health care worker) may prevent contaminating other people with the germs as well as receiving germs from others. Patients who are immune compromised often wear a mask.

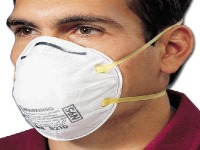
Particulate masks are also worn for airborne protection. Germs float about in the air, so masks prevent inhaling these floating germs and getting sick. Examples of floating germs include active tuberculosis (TB) as well as chicken pox. Particulate masks like the N95 mask provide a tighter mask-to-face seal so incoming / outgoing air does not leak about the nose, cheeks, and chin.
Face Shield
A
face shield or goggles are very much like a mask when it comes to standard
precautions. Using a face shield is intended to protect the nose, mouth, and
mucous membranes. Use a face shield or mask if there is a reasonable chance
that a spray or splash of body fluids may occur to the face.
Examples of procedures when face shields are typically worn include intrathecal- chemotherapy as well as injecting materials into body cavities like a subdural space.

Medical Asepsis
When we reviewed infection protection terminology we discussed medical asepsis. Here is review again.
The
term medical asepsis refers to the health care process of protecting against
infection by removing pathogenic microorganisms. Infectious agents consist of:
pathogens including bacteria, viruses, and fungi that normally live in skin as
well as mucous membranes. The health care context caters to both patients as
well as a variety of infectious agents.
Medical
asepsis involves stopping infectious agents from causing harm to patients as
well as health care workers. http://www.mercycares.com
Here are some examples of medical asepsis:
- Clean contaminated objects and (this reduces the number of organisms)
- Hand washing (this reduces the number of organisms)
- Perform disinfection as well as sterilization (this inactivates organisms)
- Use antiseptics (this inhibits organism growth)
- Medical
asepsis therefore involves reducing the number as well as the spread of
infectious agents.
For the radiation therapist, standard universal precautions for infection protection involves the use of hand washing, use of personal protective gear (gloves, gowns, masks and face shields) as well as assuring a medical environment which is disinfected so it is clean and free of contamination.
- Additional or Transmission Based Precautions
Transmission-based
precautions are employed in addition to standard / universal precautions when
using standard / universal precautions alone does not prevent the transmission
of communicable diseases. The intent of transmission-based precautions is to
eliminate or reduce the presence of pathogens ( infectious agents) in health
care settings.
So far, we have reviewed Infection Control: terminology and basic concepts, cycle of infection, as well as standard / universal precautions. We will now review clinical transmission-based case studies (hepatitis B, HIV, rubella, as well as tuberculosis) involving airborne, droplet, and contact precautions.
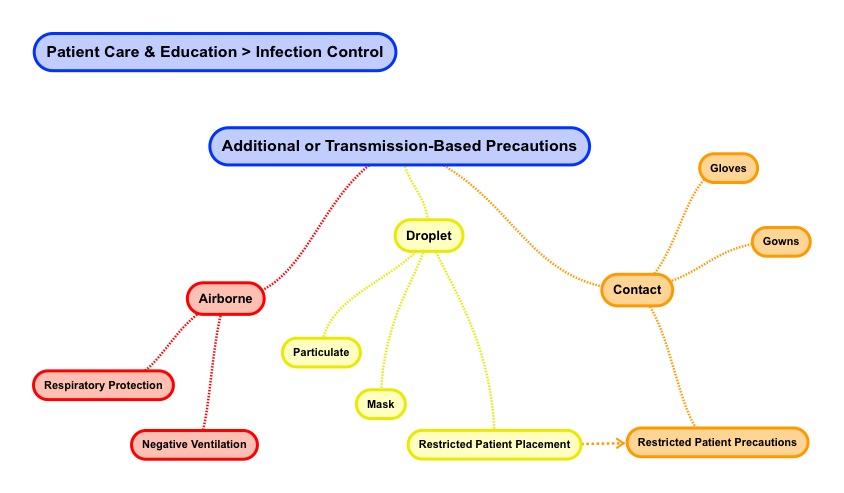
Airborne
Airborne precautions involve respiratory protection as well as negative ventilation. With regard to respiratory protection, review the use of masks in the standard / universal precautions section.
Negative
ventilation is an isolation measure used in health care. Air moves from high
pressure to low pressure areas naturally. To prevent cross-contamination among
patient rooms and from place to place in a health care setting, negative
ventilation is used in rooms designated as "isolation". For isolation
rooms, air is allowed to flow into an isolation room but air is not allowed to
escape from the room as the room air may contain an infectious agent. https://www.engr.psu.edu
Our airborne clinical transmission-based case study example is TB (tuberculosis). Tuberculosis is transmitted by airborne droplet nuclei when an infected person with TB exhales forcefully. Small infectious TB airborne droplet nuclei can easy be carried on air currents. http://www.cdc.gov/tb/
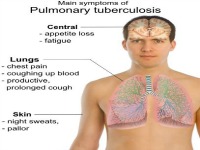
Basic transmission-based precautions for TB include: (in addition to standard precautions - gloves, gown, and face shield (as applicable))
- House the patient in an isolation (negative ventilation) restricted placement room
- Display isolation poster and educational material
- Ask the patient to wear a surgical mask
- Have health care workers wear an N95 particulate mask or respirator
- Avoid
sputum collection or aerosol inducing tests unless the patient is in a negative
ventilation room.
Droplet
Droplet precautions involve protection from infections based on droplets produced by patients talking, sneezing, as well as coughing. Droplet particles tend to be heavier than airborne particles. http://www.unc.edu With regard to droplet protection, review the use of face shield, masks, gloves, and gowns in the standard / universal precautions section.
Our droplet clinical transmission-based case study example is Rubella (German Measles). http://www.who.int/mediacentre/factsheets/fs367/en/. Rubella is transmitted by contact and droplet. Contact transmission may occur during skin rash eruptions. Droplet transmission may also occur from nasopharyngeal mucous secretions from the nose, mouth, eyes, and non-intact skin.

Basic transmission-based precautions for Rubella include: (in addition to standard precautions - gloves, gown, and face shield (as applicable))
- House the patient in an isolation (negative ventilation) restricted placement room
- Display isolation poster and educational material
- Employ airborne precaution for ~ 4 days after rash onset
- Employ
droplet precautions for ~ 1 week after rash onset
Contact
Contact
precautions involve avoiding contact with body fluids like: draining wounds,
ulcers, as well as incontinence feces. http://www.cdc.gov/hicpac/2007ip/2007ip_appenda.html With regard to
contact protection, review the use of gloves and gowns in the standard /
universal precautions section.
One contact clinical transmission-based case study example is Hepatitis B. Hepatitis B is disease, caused by a virus (HBV), may result in inflammation on the liver as well as jaundice. http://www.ccohs.ca/oshanswers/diseases/hepatitis_b.html Hepatitis B is spread by direct contact with blood as well as body fluids like mucous

Basic transmission-based precautions for Hepatitis B include:
- Immunization prior to contracting the HBV virus
- Standard
precautions to avoid direct contact with blood and body fluids
Another contact clinical transmission-based case study example is HIV (Human Immunodeficiency Virus). HIV is transmitted by contact with body fluids. http://www.mayoclinic.org/diseases-conditions/hiv-aids/basics/causes/con-20013732
The
most predominant form of transmission is by sexual contact (anal, oral, and
vaginal contact). A second method of transmission is via blood or blood product
transfusions (although this is now rare in the developed world). A third method
of transmission (relevant to health care) is via needle sticks or puncture
wound insults that take place while a medical procedure is being performed. A
fourth method of transmission is by mother-baby transfer during birth or via
breast feeding.
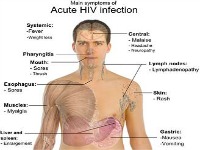
Basic
transmission-based precautions for HIV include:
- Monogamy and safe sexual contact
- Standard precautions to avoid direct contact with blood and body fluids
- Disposal of Contaminated Material
Health-care
waste consists of potentially harmful microorganisms that can infect
health-care workers, patients, as well as the general public. The disposal of
blood as well as other potentially infectious and / or hazardous material is
regulated.
The regulatory body in the United States is OSHA: the US Department of Labor > Occupational Safety & Health Administration.https://www.osha.gov In the international context, the World Health Organization has guidelines. http://www.who.int/mediacentre/factsheets/fs253/en/. Specific disposal instructions are available.
Rules
apply to: regular trash, linen, infectious waste (including pathologic),
sharps, chemo-therapeutic (chemicals, pharmaceuticals, and / or genotoxic)
waste as well as radioactive waste.
Regular Trash
Regular trash consists of products like:
- Waste paper like newspapers (documents with patient specific information must not be disposed of on regular trash) and empty glove boxes
- Food & Beverage containers

Used Linen
Linens are considered textiles that will be laundered and reused. Examples of linens used in health care are gowns and sheets. These linens may have been contaminated with infectious material and / or blood. http://www.infectioncontroltoday.com/news/2013/12/osha-confirms-that-contaminated-healthcare-linen-is-not-red-bag-waste.aspx
Used linen should be placed in an impermeable bag awaiting laundry.

Infectious Waste
Infectious
waste is waste that may be contaminated with pathogens like blood and / or body
fluids. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=INTERPRETATIONS&p_id=21010#waste
Infectious waste may also contain pathologic waste in the form of recognizable body parts. Recognizable body parts and bodies require red bag handling, incineration, as well as landfill disposal. http://weill.cornell.edu
Examples of this waste result from:
- Soiled bandages and swabs
- Used body fluid diagnostic samples
- Isolation room trash
- Used gloves and patient supplies like: IV tubing & catheters
Patient supplies are considered any item that has entered a body orifice or body. This waste is considered a biohazard and is regulated. Infectious waste must be disposed of in a close-able, leak proof red and / or biohazard bag / container.

Sharps
Sharps in the health care context consist of: needles, syringes, scalpels & lancets, injectors, as well as infusion sets.
These sharp, used / disposable supplies are considered a biohazard or contaminated with infectious microorganisms agents or gross agents like blood and / or body fluids. Sharps as infectious waste must be disposed of in a close-able, puncture & leak proof red and / or biohazard container.
To prevent (needle) stick injuries, never force sharps into a disposal container and never reach into any sharps container.

Chemo-Therapeutic Waste
Chemotherapeutic agents are drugs or medicines used to treat cancer. Chemotherapy medicines are prescribed to kill fast growing cancer cells but also affect normal cells to a lesser extent. http://www.mayoclinic.org/tests-procedures/chemotherapy/basics/definition/prc-20023578.
The treatment intent maybe to cure, control, as well as ease the symptoms of cancer growth in the body. Chemotherapeutic agents are chemical as well as genotoxic in nature. Genotoxic means that these agents are poisonous having the ability to damage DNA, cause mutations, as well as tumors. Depending on the properties of the chemotherapeutic medicine, drugs may be retained in the body some 3 to 7 days.
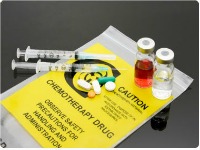
Chemotherapeutic waste must be placed in designated sealable chemical waste containers. http://depts.washington.edu
Double up on gloves if handling patient body fluids containing chemotherapeutic waste products. Observe standard / universal precautions to ensure no hazardous material gets on you or your clothing.
Home > Patient Care And Education > Infection Control
- Ethical and Legal Aspects
- Interpersonal Communication
- Patient Assessment and Management
- Treatment Side Effects
- Blood Studies
- Dietary Counseling
- Physical Assistance and Transfer
- Patient Transfer and Movement
- Assisting Patients with Medical Equipment
- Medical Emergencies
- Infection Control
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0
