Patient Assessment and Management
Home > Patient Care And Education > Patient Assessment and Management
Eight; 8 questions out of the 30 questions in the Patient Care and Education content area come from the Patient Assessment and Management sub-topic.
Can we please get your advice on this one question?
Radiation Therapy side effects can be grouped into immediate effects which occur within 2 months after radiation therapy is given and late effects that occur 6 or more months after radiation therapy. Disclaimer reminder: the discussion here is a summary review and not comprehensive so readers are encouraged to
http://www.cancer.gov/cancertopics/coping/radiation-therapy-and-you/page6
- Early Effects
Let’s begin by first reviewing immediate radiation therapy side effects that occur within 2 months after radiation therapy. Most patients experience skin changes as well as fatigue. Other side effects depend on the treatment site or body part being treated. These additional side effects may include: diarrhea, hair loss, mouth problems & swallowing issues, nausea & vomiting, sexual changes, as well as urinary & bladder changes.
- Skin Changes
Skin changes are due to radiation damaging health skin cells in the treatment area. Skin changes may include dryness, pruritus (itching), sunburn as well as peeling. Patients need to take special care of their skin during radiation therapy. This special care means being gentle with their skin, not washing off marks, as well as using mild skin soap and lukewarm water. Patients should avoid using deodorants which contain aluminum.
- Fatigue
Fatigue means being tired or weak. Fatigue is due to several radiation therapy factors among them anemia. Other fatigue factors include medications that the patient may be taking, level of activity, infection, as well as emotional factors. Fatigue is managed in several ways. Adequate rest and sleep (of 8 hours) are needed along with moderate exercise like a 15 to 30 minute walk. A patient’s work day may need to be modified to match the energy available.
There are other immediate side effects. Depending on the body site being treated patients may also have: diarrhea, hair loss, mouth problems, trouble swallowing, nausea & vomiting, sexual changes, swelling, as well as urinary and bladder changes. Most these side effects fade away after 2 months after radiation therapy.
- Diarrhea
Diarrhea is defined as frequent soft, loose or watery bowel movements. Diarrhea may occur at any time during radiation therapy. Diarrhea occurs due to irradiation to the abdomen and /or pelvis. The shaded area in the image below represents susceptible areas.
Diarrhea occurs since radiation harms healthy cells in in both the small as well as large intestines. Management is based on diet modification. Patients are advised to consume plenty of clear fluids as well as many small meals. With regard to meals, it is best if patients avoid dairy products, oily or fried foods, as well as spicy foods, A liquid and small portion bland food diet is advised for management of diarrhea.
The medical term for hair loss is alopecia. Hair loss occurs in areas irradiated since radiation damages rapidly growing cells like hair roots. Hair loss tends to occur some 2-3 weeks after the onset of radiation therapy. The use of hair products, drying as well as curling is discouraged. Common hair interventions are shaving the head as well as the use of wigs. Depending on the dose received a patient’s hair may never grow back or may begin to reappear some 3 to 6 months after irradiation. The new hair growth can be different than hair present prior to radiation therapy.
- Mouth Problems & Trouble Swallowing
Treatment to the head and neck can cause mouth problems and trouble swallowing. Radiation therapy kills as well as damages healthy cells in the mouth, airways, and lung. This radiation damage may extend to the parotid glands that make saliva and the moist linings of the mouth, airway, and lungs. The shaded areas in the images below represent susceptible areas.

Common problems include mouth sores or ulcers, infections, xerostomia, tooth loss and / or tooth decay, thick saliva, stiffness, as well as loss of taste. Swallowing troubles tend to appear some 2 to 3 weeks after the onset of radiation and tend to resolves some 4 to 6 weeks after treatment. Throat changes may relate to throat soreness as well as trouble swallowing due to irradiation of the epiglottis. Mouth sores tend to go away after radiation therapy treatment. Taste issues as well as xerostomia may resolve after several months or may remain permanent. Proactive management involves the patient visiting a dentist and/or dietician prior to treatment. Patients need to practice good oral cleaning hygiene, keep their mouths moist, eat small meals avoiding sugars, tobacco, & alcohol, engage in regular jaw exercise, as well as regularly following up with dentists and/ or dieticians.
Radiation therapy to portions of the small intestine, large intestine, colon, as well as parts of the brain can cause nausea and vomiting. Nausea is feeling sick to your stomach while vomiting involves dry heaves and throwing up. The shaded area in the image below represents susceptible areas.

Of course, the onset & severity of nausea as well as vomiting depends on the dose as well as areas irradiated. Nausea and vomiting tend to occur some 30 minutes to hours after radiation therapy. Management for nausea and vomiting involves having patients adopt a bland foods low residual diet. The consumption of 5 to 6 smaller snacks or meals rather than 3 larger meals is suggested. Patients are encouraged to plan the times of meals to avoiding consumption before as well as after proximity to treatment times.
Sexual changes including fertility changes may take place after radiation therapy to the pelvis. Pelvic radiation may cause tissue scaring based on the dose as well as location of irradiation. Changes also include hormonal changes and are different for men and women. For men, sexual changes may mean erectile dysfunction and the inability to father children. For women, sexual changes may mean uncomfortable sex, vaginal dryness, vaginal stenosis, menopause, as well as the inability to bear children. The shaded areas in the images below represent susceptible areas.

Most people would like to maintain the same sexual life they had before undergoing radiation therapy. Management includes patient education. The objectives of patient education are: to understand side effects (fertility, impotence, and sex) prior to therapy, couple counseling, as well as planning. An honest discussion between a patient and their partner(s) about radiation therapy consequences is encouraged. In applicable cases a patient’s sperm or eggs can be banked for later use ahead of radiation therapy.
Urinary and Bladder changes may take place after radiation therapy to the pelvis. Pelvic radiation may cause tissue cystitis (inflammation), ulcers, and infection based on the dose as well as location of irradiation. Issues may include painful urination, difficult emptying the bladder, incontinence, blood in the urine, as well as spasms. The shaded area in the image below represents susceptible areas.

Symptoms may begin some 3 to 5 weeks after the onset of radiation therapy and tends to resolve some 2 to 8 weeks after the end of treatment. Management stresses diet counseling. Patient are advised to drink 6 to 8 glasses of water and consume a diet free of alcohol, caffeine, spices, as well as tobacco. In cases of painful urination, infection, blood in urine, as well as spasms medications are prescribed for the management of symptoms.
Late side effects begin 6 months or more after radiation therapy is over. These late side effects depend on the body site treated as well as the radiation dose received. Some late side effects are: brain changes, lymphedema, infertility, xerostomia, joint problems, as well as secondary cancer. We will discuss three late side effects; namely, brain changes, lymphedema and joint problems.
- Brain Changes
When the brain receives radiation therapy changes may occur some months to years after therapy. Brain cells dying and forming a mass is called brain necrosis. Some late brain effects may be memory loss, visual changes, trouble thinking, as well as personality changes. Management of brain necrosis includes counseling, medications, as well as surgery.
- Lymphedema
Lymphedema is the build-up of lymph fluids which results in swelling examples like arm swelling or leg swelling. Lymphedema occurs due to the removal of lymph nodes during surgery and / or the damage of lymph nodes by radiation. Limb heaviness, swelling, and redness are early signs of lymphedema. Management for lymphedema prioritizes physical activity over a sedentary lifestyle. Compression wraps as well as care for the extremity in terms of clothing to manage environment exposure is recommended.
- Joint Problems
Weakness as well as scar tissue may result from radiation therapy to joints. The onset of joint problems may occur some months after radiation therapy. Stiffness on movement as well as limited joint range of motion may be signs of joint problems. Management takes the forms of: exercise and physical therapy.
An understanding of blood studies allows the Radiation Therapist to better appreciate a patient’s condition
Radiation Therapy can reduce white cell count as well as reduce platelet levels. Blood assists the body to fight infection as well as prevent bleeding. Some of the other factors which can affect the blood values of Cancer patients are chemotherapy as well as intravenous contrast a patient may receive as part of their radiation therapy simulations procedure.
- CBC
The complete blood count (CBC) is a commonly ordered blood test. The major portion of this blood study measures the concentration of white blood cells, red blood cells, as well as platelets in the blood.
White blood cells are part of the body’s immune system and assist the body in fighting infections. A low white cell count may be a response to chemotherapy. While a high white cell count may signify an infection or malignancy in the body.
Red blood cells carry hemoglobin which is responsible for oxygen transport in the body. A low red blood cell levels may signify anemia. While a high red blood cell count may be a response to bone marrow disease or hypoxia (low levels of blood oxygenation).
Platelets are colorless disk shaped blood cell fragments responsible for clotting. A low platelet count may mean a patient has a difficulty clotting. While a high platelet count may signify inflammation or a bone marrow problem.
- BUN
Another common blood study is: blood urea nitrogen or BUN. BUN levels reveal information on how well a patient’s kidneys as well as liver are working. Here is a basic idea of how the body forms as well as gets rid of urea nitrogen. Our livers produce ammonia which contains nitrogen. Nitrogen combines with oxygen, carbon, as well as hydrogen in the blood to form urea. Urea is filtered by our kidneys and leaves the body through urine. A BUN (blood urea nitrogen) blood study reveals if urea nitrogen levels are higher than normal which may mean a patient’s kidneys and liver may not be working properly.
- Creatine
Creatine is another common blood study. Creatine is found in most body tissue and is responsible for supplying energy for muscles. Creatinine is a waste product from creatine. Creatine levels reveal how well a patient’s kidneys are working. Normal kidneys are capable of efficiently removing creatine from the blood. If creatine levels rise it may mean that kidney function is compromised.
A patient’s iodine allergy status, BUN / creatine levels are routinely checked before administering iodine based intravenous contrast for a patient Cat Scan radiation therapy simulation procedure. The Radiation Oncologist ordering the simulation will establish guidelines for contrast administration. http://middlesexhospital.org/our-services/hospital-services/radiology/for-physicians-online-ordering-manual-and-information/ct-ordering-guide
- GFR
Glomerular filtration rate or GFR is yet another blood study used to check how well a patient’s kidneys are functioning or index kidney function. The GFR blood study measures the how much blood filters through a patient’s kidney glomeruli each minute. GFR values are often considered before administering intravenous MRI gadolinium contrast. Factors affecting how blood values are read include a patient race, age, as well as gender. A patient’s weight is also considered before determining the amount of contrast material to administer.
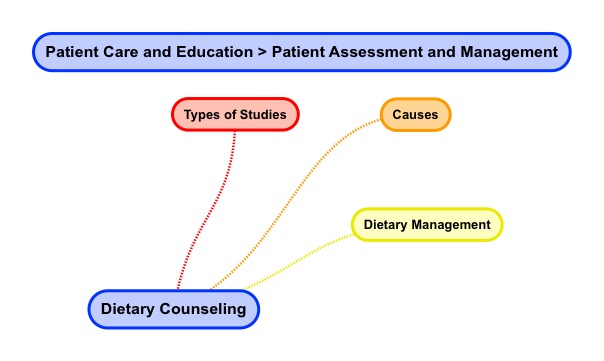
- Dietary Counseling
Dietary counseling is important. Providing nutritional support during radiation therapy is part of a patient’s assessment as well as management. Dietary counseling for Cancer patients certainly improves their quality of life outcomes.
http://www.ncbi.nlm.nih.gov/pubmed/15684319
Not all patients will require the same nutritional interventions and/ or dietary counseling. The side effects of radiation therapy depend on the site as well as volume being irradiated, the total dose and fractionation. Patients receiving radiation therapy to the head & neck or any aspects of the gastrointestinal tract are more likely to face nutritional related radiation therapy side effects. Dietary counseling to a great extent is based on symptom management and addresses an individual patient’s nutritional situation.

Some of the diet-related treatment side effects for patients receiving radiation therapy to the head & neck include: pain on swallowing, taste changes, xerostomia, as well as nausea and vomiting. Some of the diet-related treatment side effects for patients receiving radiation therapy to the gastrointestinal tract involve anorexia (loss of appetite), diarrhea as well as enteritis. Gastrointestinal treatment side effects are due to the interference with ingestion, digestion, as well as the absorption of ingredients.
Diet issues may begin during the second to third week of radiation therapy treatment and extend two to three weeks after therapy. Some side effects may become chronic; continuing after radiation therapy ends. Weight loss, protein wasting, or malnutrition are secondary to a patient’s inability to intake foods and are common.
Nutritional counseling as well as diet modification are important to maintain a patient’s intake, weight status, as well as quality of life. Patients with good nutrition are more likely to tolerate the side effects of treatment. Indeed, tumor-induced effects on nutritional status are well known.
http://www.cancer.gov/cancertopics/pdq/supportivecare/nutrition/HealthProfessional/page2
A variety of nutritional interventions are available from tube-feeding and nutritional shakes thru a low residual diet. Tube-feedings overcome a patient’s inability to swallow. Residue in a diet refers to undigested foods. The idea behind a low-residue diet is to reduce the number as well as the size of bowel movements patients may have each day.
Here are some common dietary counseling recommendations. Patients are encouraged to plan meals in advance, eat small frequent meals every two hours, consume a third of calorie requirements at breakfast, and consume foods that appeal to their sense of smell.
Patients are encouraged to eat more green & colorful fruits and vegetables, whole grains, nuts, seeds, and fish. Patients are discouraged from consuming processed foods with preservatives, simple sugars, alcohol, and tobacco.
Home > Patient Care And Education > Ethical & Legal Aspects
- Ethical and Legal Aspects
- Interpersonal Communication
- Patient Assessment and Management
- Treatment Side Effects
- Blood Studies
- Dietary Counseling
- Physical Assistance and Transfer
- Patient Transfer and Movement
- Assisting Patients with Medical Equipment
- Medical Emergencies
- Infection Control
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0